

MOC Frequently Asked Questions
A diagnosis of cancer is never easy to hear. This is especially true when you learn you have a rare type, such as mucinous ovarian cancer (MOC).
Dr. Jennifer Mueller, a surgeon at Memorial Sloan Kettering Cancer Center in New York and an Coalition Advisory Committee member, answers the mostly commonly asked questions about MOC.
Q: What is so different about
mucinous ovarian cancer?
A: A primary mucinous ovarian cancer—MOC—is an uncommon type of ovarian cancer and accounts for less than 3% of the so-called ‘epithelial’ ovarian cancers.
It is very important to mention that ‘epithelial’ ovarian cancers include many different cell types, not just mucinous. So, it can be challenging to try to do research about MOC on your own, because most of the resources you come across will give information that is not specifically related to mucinous ovarian cancer. That’s why it is so important to have an expert health care team unpack your questions and make sure you have the facts.
Over two-thirds of women with MOC are diagnosed at an early stage (stage 1). This means the cancer is limited to just the ovary and has not spread to any other organ in the body. Women with MOC have an overall better prognosis than women with the more common ‘high-grade serous’ ovarian cancer type. We think this is because more women with MOC are diagnosed at an early stage.
About one-third of women with MOC are diagnosed with more advanced stages of disease. This means the cancer has spread beyond the ovary to other parts of the body. Advanced stage MOC is harder to treat, partly because it does not respond as well to chemotherapy drugs.
For this reason, oncologists often take an aggressive approach in treating advanced stage disease, using a combination of surgery to remove all the visible cancer, and chemotherapy, to kill cancer cells that the surgeon may not be able to see.
Q: Is there more than one type
of MOC?
A: Most MOCs actually aren’t primary ovarian cancers. The more common situation is that a mucinous cancer, found in a woman’s ovary, started in another place in her body. Most of the time these cancers come from the gastrointestinal tract, and less commonly from the pancreas, cervix or breasts.
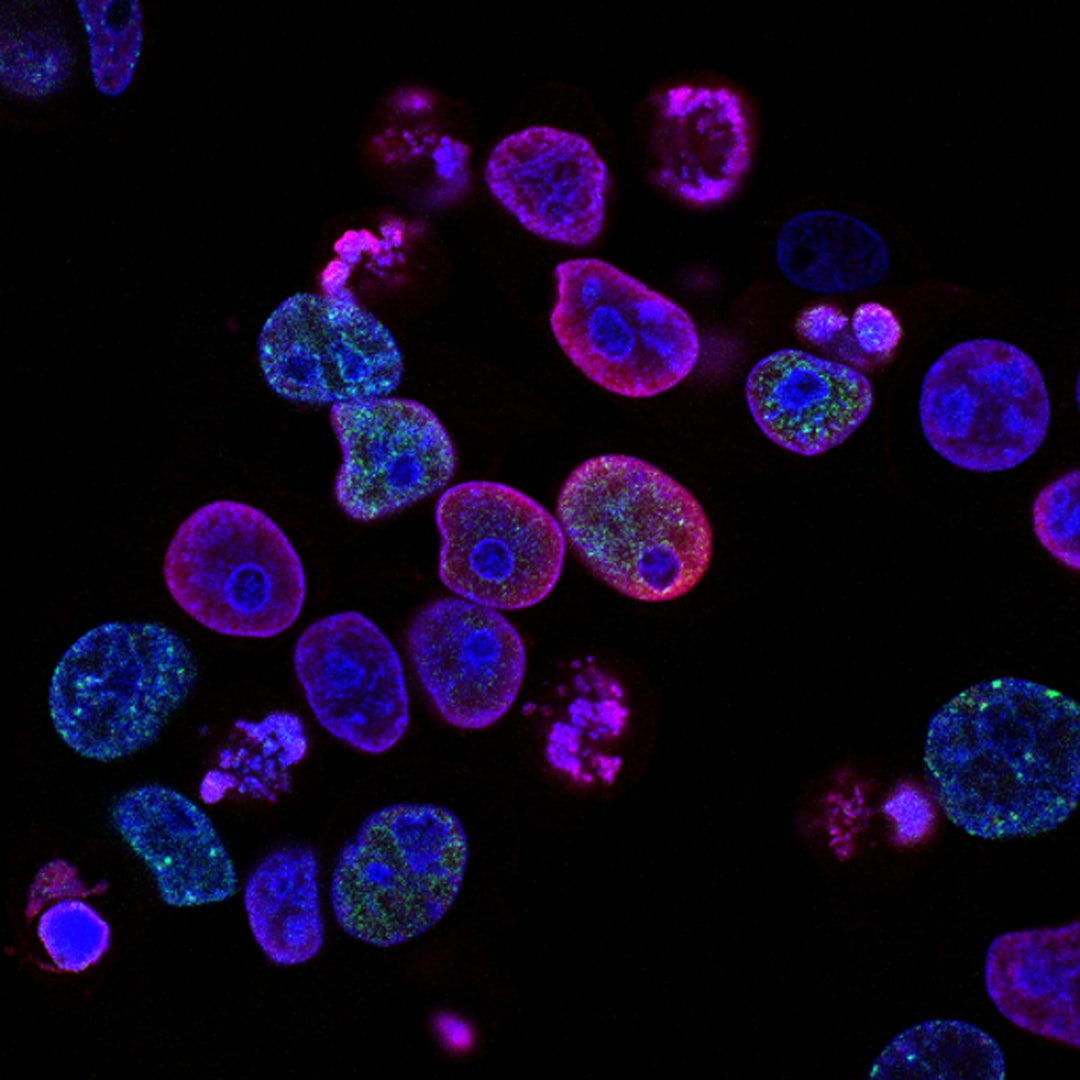
In this situation the cancer is not primary to the ovary—meaning that it didn’t start there. Instead, it is called an ovary metastasis--a cancer that started somewhere else and spread to the ovary. Sometimes pathologists can tell whether a mucinous ovarian cancer is primary or metastatic based on the appearance of the cancer cells under the microscope.
Doctors use imaging (usually a CAT scan), the pathology report, and tumor markers that can be measured in the blood (CA-125, CEA and CA19-9) to help determine whether a cancer is primary or metastatic. It is very important to have a thorough evaluation looking for cancer in other areas of the body.
These tests can be done before or after surgery and include colonoscopy and upper endoscopy to examine the lining of the digestive system, mammogram to examine the breasts, a cervical pap smear, and physical exam that includes a pelvic exam.
